Alpha Medical closes $24M Series B round to expand women’s telehealth — without the video calls
Alpha Medical, a telemedicine company focused on women’s healthcare, closed a $24 million Series B round on Tuesday. It’s another company situated squarely in the crosshairs of a pandemic-fueled boom in telemedicine investment, though Alpha Medical’s approach has one notable difference: you won’t be logging on to any Zoom calls.
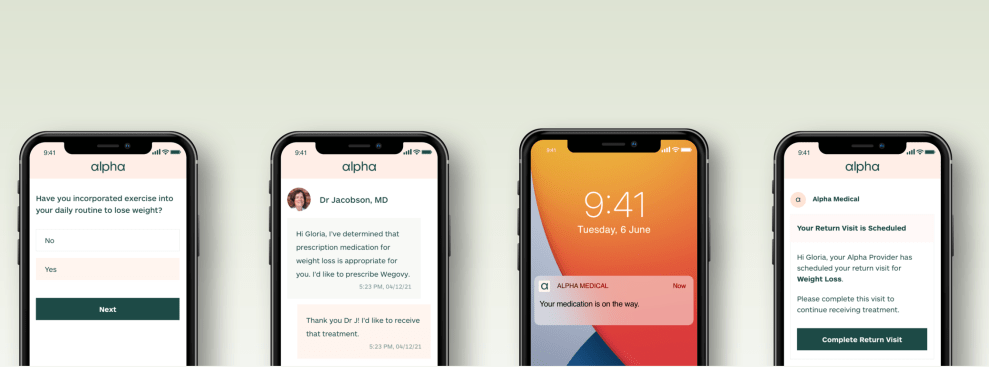
Alpha Medical was founded in 2017. Since then, the company has created a network of 30 staffed primary care providers (PCPs in industry shorthand), who treat female patients online, without phone or video calls. For a $120 yearly fee (not covered by insurance) you can make an account, supply your medical history and patient intake forms, and are assigned a PCP with whom you’ll communicate via an online platform.
This type of telehealth is sometimes called “store and forward” — patient health records can be viewed by a physician on an online platform, rather than during a real-time visit.
“We give you a primary care physician who is fluent [in women’s health],” co-founder and CEO Gloria Lau tells TechCrunch. “We do all of this online, asynchronously.”
There are exceptions to this; you might be referred to a lab for testing, or to another primary care provider if a condition can’t be managed online. “But when you look at the grand scheme of things, we think about 80% of stuff can be done online. The remaining 20% or so needs to be in person,” Lau says.
Alpha’s new funding may not be a mega-round, but it fits within the trend. It brings the company’s total funding to $35 million, counting a Series A round that gleaned about $11 million. It includes participation from SpringRock Ventures, Margo Georgiadis, Outcomes Collective Growth Capital, FMZ Ventures, Samsung Next, Chamaeleon, AV8 Ventures and GSR Ventures.
The previous round of funding helped the company accelerate its coverage: the company grew from offering services in about 10 states to 46, including D.C., Lau estimates. It also helped the company increase the number of conditions its providers can manage, from about three to 60.
This new round will allow the company to train and locate providers who can manage even more conditions (the most recent addition was polycystic ovarian syndrome). It will also allow the company to expand from direct to consumer services to B2B services.
“We’ve started talking to health plans and employers to bridge the gap,” says Lau. “We’re in lots of conversations with health plans, we have some very small employer contracts that are inbound — actually that’s how we started thinking about it in the first place.”
Lau is one of Alpha Medical’s two co-founders, and her expertise is primarily in the data world. She’s a consulting faculty member at Stanford Engineering and a former vice president of Data at Timeful, which was acquired by Google in 2015. The clinical expertise informing Alpha medical comes from Lau’s chief medical director Mary Jacobson, an obstetrician and gynecologist.
Alpha Medical is hoping to fill a growing gap in primary care service. And there’s evidence that a lack of primary care is a pressing problem. The Health Resources and Services Administration has designated about 3,434 medically underserved areas — meaning these areas are experiencing a shortage of primary care providers. A total of 14 million people live in those medically underserved areas.
The existence of these “primary care deserts” has long been a selling point for DTC telehealth companies. Companies like Ro, now valued at $5 billion, just boasted of reaching patients in 98% of such deserts, by its own calculations.
The Alpha Medical user is also a woman who lives somewhere without a plethora of PCPs. But that’s just one piece of the puzzle. Alpha’s target demographic also includes people with high deductible health plans, or people with no insurance at all, says Lau.
Even among people with insurance in places with primary care available, there’s some evidence that primary care visits are declining. A 2021 study published in “The Annals of Internal Medicine” analyzed 142 million primary care visits among people who had insurance between 2008 and 2016. The study found that primary care visits had declined 24.2%, while visit rates to specialists remained stable. The decline was greatest among young adults.
The study outlined a few factors driving the decline. Higher costs (the average out of pocket cost rose from $29 to $39 over that time period), high deductibles, lack of access to care and the fact that people might be visiting urgent care clinics or specialists instead.
Alpha Medical’s services aren’t currently covered by insurance — but Lau offers that the $120 per year price for all visits is sufficiently affordable to entice people who already pay for high deductible health plans or those who are uninsured. There’s also an à la carte feature of the service, where a visit costs anywhere from $15-$30.
The average income for an Alpha Medical user, Lau says, is about $40,000 per year. That’s somewhat aligned with the median income for women working full time, per the 2020 census: about $47,300 per year.
“The reason why we can be so affordable is because it’s asynchronous,” says Lau. “You’re not paying for the time while the doctor is waiting for you to think about your symptoms or your family history. We only notify the clinician when all the information is collected in the system, [and] integrated in the EMR [electronic medical record].”
The idea of asynchronous healthcare might feel a bit strange at first glance. One of the biggest advantages of having a primary care doctor is having a personal relationship with a healthcare provider.
But if there was ever a time to fuse telehealth and women’s healthcare, now might be the time.







